Active surveillance is a conservative management approach that is increasingly being used for patients with low- and intermediate-risk prostate cancer.

Englman
"With active surveillance, patients are closely followed up to identify if and when cancer progression occurs," said Cameron Englman, MD, a clinical research fellow and PhD student in the Imaging Department at the University College London Hospital (UCLH). "Unlike active treatment, active surveillance avoids unnecessary treatment for clinically localized disease and identifies progression to trigger deferred procedures without losing the window of curability."
With this in mind, one has to ask, why aren't more health care providers – and patients – pursuing active surveillance?
"To work, patients must comply with the active surveillance follow-up protocol, which has proven to be challenging," added Dr. Englman, who made his remarks during a Wednesday session.
Improving Compliance Starts with Decreasing the Burden
Active surveillance usually involves a combination of serial prostate-specific antigen (PSA) tests, digital rectal exams, imaging and prostate biopsies.
"It's the latter, which can be invasive, uncomfortable and have significant side effects, that tends to be the reason many prostate cancer patients decide to discontinue surveillance," Dr. Englman said.
Thus, it stands to reason that to improve compliance, one must first decrease the burden—and that means reducing the frequency of biopsies. This is where MRI could help.
The Benefits of MRI Monitoring
A recent UCLH study suggests that patients on active surveillance can be safely monitored with MRI, with the decision to biopsy being based on imaging findings and PSA kinetics.
The study was based on an MRI-led active surveillance cohort run by UCLH.
"The central strategy of this cohort was not to perform predetermined biopsies, but to base follow-up on PSA and MRI, with further sampling only in cases of radiological change or unexplained PSA fluctuations," Dr. Englman explained.
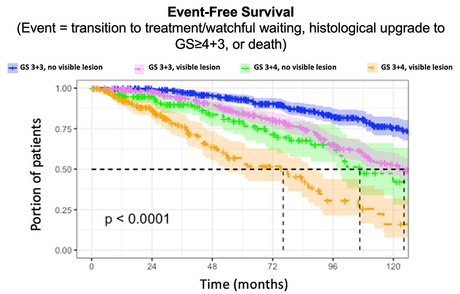
The rates of survival and initiation of treatment of the MRI-led active surveillance cohort, which includes over 1,100 patients, are comparable with published data from surveillance cohorts following mandated protocol-based biopsy. Furthermore, the UCLH cohort dropout rate is less than 1%—significantly lower than the 25% rate for patients with stable disease on normal surveillance.
More MRI Could Mean Less Biopsies
According to Dr. Englman, this data indicates that, by expanding the role of prostate MRI, active surveillance can be delivered without the need for regular, intrusive biopsies.
"With regular MRI, prostate biopsies based on predetermined intervals may not be necessary for active surveillance, which could increase compliance and decrease patient drop-out," Dr. Englman concluded.
The UCLH research team also found that patients with a visible prostate cancer lesion on MRI were more likely to have worse clinical outcomes, meaning they could require more biopsies yet gain less benefits or even die quicker than patients with no MRI-visible lesion. This too could help reduce the number of intrusive, but ultimately unhelpful, biopsies.
Based on this research, UCLH is now working to develop a personalized risk-stratified approach to active surveillance.
Access the presentation, "Magnetic Resonance Imaging-Led Active Surveillance for Prostate Cancer: Outcomes From a Large Cohort Study," (W3-SSGU05-3) on demand at Meeting.RSNA.org.