By Melissa Silverberg
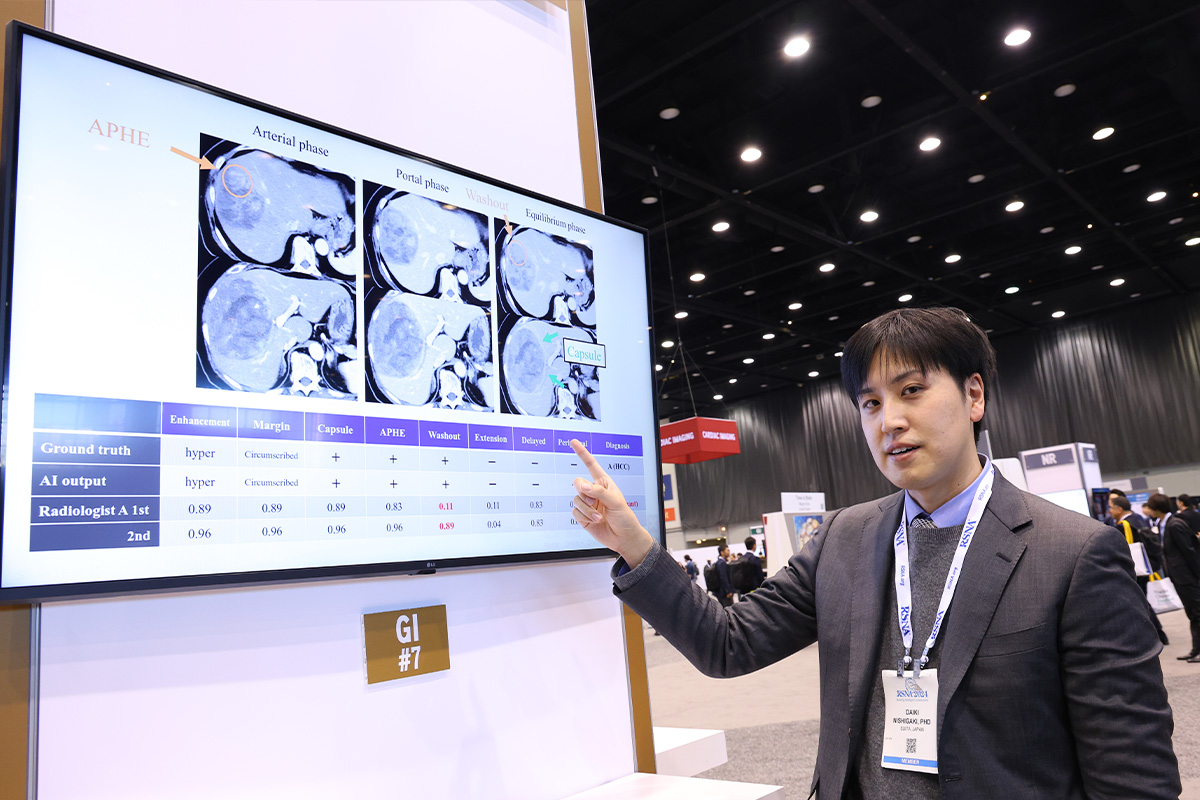
Using AI can improve radiologists’ performance in characterizing and diagnosing hepatic lesions, according to an analysis presented on Sunday by Daiki Nishigaki, MD, Osaka University Graduate School of Medicine in Japan.
AI can be used to evaluate image features across all hepatic lesions and produce outputs that can boost diagnostic confidence when there are no conflicting findings. However, if any features do not match the typical findings, AI can provide radiologists with an alert indicating a potentially atypical case.
With the rapid advancement of AI, Dr. Nishigaki is most interested in how to become a radiologist whose work is enhanced by AI rather than afraid of the new technology, particularly for identifying these lesions and assisting with earlier diagnosis.
To investigate the performance of radiologists in characterizing and diagnosing hepatic lesions with and without the assistance of AI, a retrospective study included 83 nodules or masses from 69 patients who underwent dynamic contrast-enhanced CT of the liver. Image assessments were conducted by 20 radiologists grouped according to their level of experience (10 senior and 10 junior).
Each radiologist determined the probability of eight characteristics based on enhancement patterns and the diagnosis with and without AI. After assessing the characteristics of a lesion, the readers placed it into one of the following four categories: (a) classic hepatocellular carcinoma (HCC); (b) malignant liver tumors other than classic and early hepatocellular carcinoma; (c) indeterminate lesions on imaging; or (d) benign lesions including hemangiomas and perfusion alteration.
Their results were compared with a reference standard determined by two board-certified abdominal radiologists.
“We discovered that using AI can enhance both the performance and consistency of radiologists' image interpretations, regardless of their years of experience,” Dr. Nishigaki said.
While the results were not unexpected, Dr. Nishigaki did note two findings that were encouraging.
“First, the improved diagnostic performance for HCC when using AI, and second, its usefulness even for experienced senior radiologists, both of which support previous studies,” Dr. Nishigaki said. “Additionally, while previous research had not reported this, our results showed that accurately evaluating imaging characteristics with AI directly led to better diagnostic performance of radiologists, which has significant implications for our daily workflow.”
The findings reinforce the importance of detailed imaging and contribute to the understanding of how AI can help the radiologist perform their job even better, leading to better patient outcomes.
“We expect that detailed AI-based analysis of hepatic tumors will aid in predicting prognosis and treatment efficacy, potentially leading to the discovery of new imaging biomarkers,” Dr. Nishigaki said.
Access the poster, “Performance of Radiologists in Characterizing and Diagnosing Hepatic Lesions Using Dynamic Contrast-Enhanced CT With and Without Artificial Intelligence,” (S3A-SPGI-7) on demand at RSNA.org/MeetingCentral.
© 2024 RSNA.
The RSNA 2024 Daily Bulletin is the official publication of the 110th Scientific Assembly and Annual Meeting of the Radiological Society of North America. Published online Sunday, December 1 — Friday, December 6.
The RSNA 2024 Daily Bulletin is owned and published by the Radiological Society of North America, Inc., 820 Jorie Blvd., Suite 200, Oak Brook, IL 60523.